Falls are the leading cause of injury among Canadian seniors
Every year, 20–30% of seniors fall at least once.
Falls are responsible for 85% of injury-related hospitalizations in seniors and 95% of all hip fractures, and have direct estimated costs of over $2 billion.
Over one-third of elderly persons hospitalized after a fall are taken in by a long-term care establishment (CHSLD) upon their release from hospital.
Falls can lead to chronic pain, reduced mobility, loss of autonomy and even death.
It is noteworthy that 50% of falls leading to hospitalization occur at home.
Source: Report
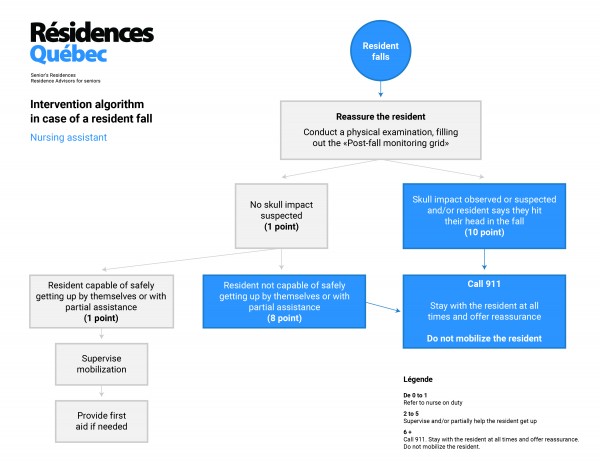
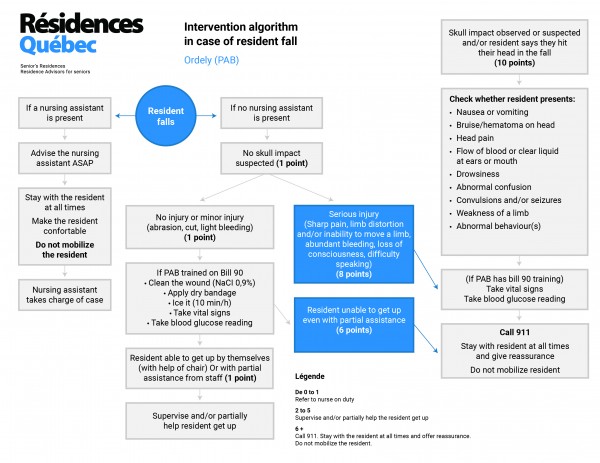
Private residences (RPAs) have developed procedures to follow if a resident falls:
- A procedure for orderlies (PABs) if there is no nurse on the floor
- A separate procedure for nursing assistants
Falls are difficult to prevent. They happen, be it at home or in RPAs.
The reason for a senior falling can vary:
- Drop in blood pressure
- Chronic illness, acute conditions or other degenerative diseases
- Malnourishment, anemia
- Ill-adapted environment, e.g., slipping on a wet bathtub surface or loose rug
- Degenerative diseases such as dementia or Parkinson’s
- Ill-suited medication
- Cluttered rooms
- Balance or gait deficiencies
- Poor nutrition
- Social isolation: seniors living alone have higher fall rates
The risk of falls and injury from falls is two to three times higher in seniors with dementia or other cognitive impairment.
Mental confusion and disorientation, which can also manifest as delirium, also increase the risk of falling. Delirium can be caused by acute infection, medications, dehydration, sensory impairment or emotional distress.
Seniors with visual impairments are 2.5 times more likely to experience falls.
- Muscle weakness and decrease in physical fitness: Loss of muscle strength and endurance can reduce a person’s ability to recover when they slip or trip. The risk is four to five times higher.
- Acute illnesses: The symptoms of acute illness, including weakness, pain, fever, nausea, dizziness, can increase the risk of falling.
- Infections, especially those of the urinary tract, are a triggering factor in 8% of falls.
In addition, the effects of drugs taken to treat diseases or symptoms can also increase the risk of falling.
- Assistive devices: These devices can promote autonomy and mobility, while also preventing falls, if they are used properly and suitably maintained. However, lack of maintenance, defects, poor adjustment and over-dependency on the device can turn it into a potential cause of falls. Cane tips can wear out, wheels of walkers and wheelchairs can loosen and assistive devices may be too heavy or the wrong size.
- Shoes and clothes: Inappropriate shoes (thick soles, slippery straps, high or narrow heels) have been associated with fall risks. Overlong clothing can hinder walking and slippery fabrics like satin can cause a senior to slide off their seat. Additionally, clothing that is difficult to put on can lead to a person with reduced mobility losing their balance and falling while dressing.
- Risky behaviours: For an elderly person, behaviours like walking without the walker or cane they depend on can result in falls and injury.
- Excessive alcohol: Alcohol can interact with certain medications and increase the risk of falling by altering perception, balance and gait.
- Poor nutrition: It is reasonable to expect that dehydration and malnutrition due to eating poorly and not drinking enough can lead to muscle weakness, fatigue and frailness.
- Fear of falling: The fear of falling is in itself an important risk factor for falls. A recent analysis of data on Canadian homes revealed that 34% of Canadians aged 65 or over are afraid of falling. This fear can lead to reduced physical activity, which then leads to muscle weakness and poor balance.
- Medication: Some studies have highlighted a strong correlation between falls and fractures in seniors and certain drugs, particularly psychotropics (which affect mood), tranquilizers and sleeping pills. These include benzodiazepines, antidepressants and antipsychotics.
Any medication that can cause sleepiness, dizziness, low blood pressure, Parkinsonian symptoms, ataxia, or gait or visual disturbances increase the risk of falls in the elderly.
In addition, medications that reduce bone density or increase the risk of bleeding can increase the likelihood of injury during falls and the seriousness of those injuries.
- Vitamin D: Vitamin D is associated with bone and muscle strength.
Researchers recently established that taking a vitamin D supplement (with or without a calcium supplement) reduces fall risks.
Measures to help prevent falls:
- Better ratio of care staff for seniors in all types of residences
- Peer program (daily prevention calls with alert in case of non-confirmation)
- Emergency ringers or pulls
- Surveillance cameras
- Fall monitor cushions
- Technical assistance or mobility aids: e.g., walkers, canes, etc.
- Call bracelets or necklaces
- Exercise!
Source: Government of Canada
Need help?
Contact a residence advisor to help you in your search for a residence
844 422-2555
Service free of charge for beneficiaries
Member of ACHQ
Need help?
Contact a qualified residence advisor for help with your search and accompany you until the signing of your lease for FREE.
Our assistance service for the elderly is FREE*
844 422-2555
* Our residence advisors are paid by the network of private residences in Quebec certified by the Ministry of Health and Social Services.